Understanding Biofilm in Healthcare Cleaning
Understanding Biofilm in Healthcare Cleaning
Biofilm is a common but often overlooked challenge in healthcare settings, where it can increase the risk of infections. Understanding what biofilm is, how to recognize it, and how to remove it effectively is essential for healthcare environmental services staff.
What is Biofilm?
Biofilm is a slimy layer of microorganisms like bacteria, fungi, and other germs that stick to surfaces and protect themselves with a glue-like coating called extracellular polymeric substances (EPS). This coating shields the germs, making them harder to clean and kill compared to germs that are floating freely.
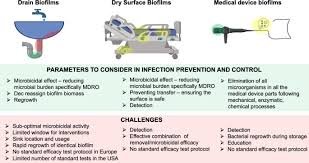
Biofilm can grow on any surface that stays damp, including medical equipment, floors, walls, sinks, drains, pipes, and high-touch areas like bedrails or counters. The National Institutes of Health (NIH) estimates that 80% of microbial infections are associated with biofilm, making its removal a top priority in healthcare cleaning.
Why is Biofilm a Problem in Healthcare?
Biofilm is a serious concern in healthcare because it is resistant to cleaning and disinfection, often hard to detect, and can harbor dangerous germs that spread infections. The slimy coating protects germs, making them up to 1,000 times more resistant to disinfectants and antibiotics. Biofilm can form in cracks, drains, or beneath hard-to-reach surfaces, which can contribute to the spread of healthcare-associated infections (HAIs).
How to Recognize Biofilm
Biofilm can sometimes be visible as slimy, sticky, or greasy layers on surfaces. Dull or discolored areas, particularly in places that remain wet, can also indicate biofilm. A musty or foul odor is another clue. In cases where it is not visible, tools like fluorescent dyes, ATP testing, and magnification devices can help detect biofilm in hidden or hard-to-see areas.
The Association for the Healthcare Environment (AHE) emphasizes the importance of routine inspections and testing for biofilm, especially in high-risk areas like drains or equipment.
How to Clean and Remove Biofilm
Removing biofilm requires more than standard cleaning methods. It involves multiple steps to ensure the biofilm is fully broken down and removed:
1. Physical Removal: Use brushes, microfiber cloths, or mechanical systems like automated washers to physically scrub and break up the biofilm layer.
2. Chemical Cleaning: Apply enzymatic cleaners or surfactants to dissolve the slimy coating. Follow with an EPA-registered disinfectant effective against biofilm, such as hydrogen peroxide, sodium hypochlorite (bleach), or peracetic acid. Be sure to allow the disinfectant to sit for the recommended contact time to fully penetrate the biofilm.
3. Rinse Thoroughly: Rinse surfaces with clean water to remove chemical residues and loosened particles.
4. Dry the Area: Moisture promotes biofilm growth, so ensure surfaces are dried thoroughly using clean towels or ventilation systems.
5. Monitor and Maintain: Regularly inspect and clean high-risk areas to prevent biofilm regrowth. Use ATP testing or other tools to ensure cleaning efforts are effective.
Preventing Biofilm Formation
Prevention is key to minimizing the risks associated with biofilm. Steps to prevent biofilm formation include:
• Keeping surfaces dry by fixing leaks and eliminating standing water.
• Cleaning and disinfecting high-risk areas daily, using products specifically designed for biofilm management.
• Treating surfaces with anti-biofilm coatings to make them less hospitable for microorganisms.
• Disassembling and thoroughly cleaning equipment, especially in damp areas or hidden crevices.
• Training staff on biofilm prevention and removal techniques to ensure best practices are followed.
AHE recommends regular education and training for cleaning teams to stay ahead of biofilm-related risks in healthcare facilities.
Why Biofilm Cleaning Matters
Biofilm is not just a cleaning problem; it is a serious health risk. Effective biofilm management protects patients, prevents infections, and ensures healthcare facilities remain safe and hygienic. For more information, consult trusted resources like the Association for the Healthcare Environment (AHE) and the National Institutes of Health (NIH), which offer expert recommendations on biofilm management.